Medical billing utilizes Accounts Receivable as a core business concept that handles outstanding financial obligations in the healthcare revenue cycle. This represents unpaid healthcare provider bills from services delivered to both patients and insurance organizations. The AR system tracks the payment process after medical service providers present their bills to patients or insurers. Healthcare providers need a well-functioning AR process to manage their financial operations by securing sustained revenue flow, lowering payment delays, and decreasing their financial exposure.
What Is AR In Medical Billing
Medical billing functions depend heavily on accounts receivable because this system serves as an indispensable component. The provider considers A/R as payment expected from patients after delivering medical services. The correct handling of A/R operations maintains financial stability and operational capability for medical businesses. The article provides detailed information about medical billing accounts receivable functions together with their medical practice value while offering appropriate management methods.
What is AR Days In Medical Billing
AR Days represent the timeframe that medical practices need to collect unpaid bills submitted to insurance companies on behalf of their insured patient claims. The measurement includes payments from both patients and insurance companies with three calculations at 3-month, 6-month, and 9-month intervals.
Practices with financial difficulties often experience AR days exceeding 50 days while the standard metric falls within a 30 to 70 day period. Calculating AR days serves to determine the earliest possible payment dates for bills and claims so excessive time beyond 50 days indicates performance issues which result in AR stress for your practice.
How to Calculate AR Days?
It is essential to determine your practice’s AR days because a thorough assessment of billing performance depends on this information. To determine AR days, your practice needs to use this calculation formula:
A/R Days = (Accounts receivable ÷ Annual revenue) x Number of days in the year
The calculation works as follows, yet requires your practice to identify its daily revenue amount before application. Start by adding all charges that your service has posted during the selected timeframe before subtracting credits that have been received in return for these charges. The period duration for which you selected obtains grounds for breaking the final number into AR days. This quantity then serves as the value for the formula stated earlier.
You have receivables of $80,000 alongside Gross charges of 700,000, but you also have a credit balance of $10,000. To find the result, use this mathematical sequence:
The formula for determining receiver cash flow performance involves dividing the difference between total receivables and credit balance by the average daily gross charge amount, which equals gross charges divided by 365 days.
($80,000-$10,000)/ ($700,000/365 days)
$70,000/1917 = 36.91 AR days
AR Follow Up In Medical Billing
To achieve successful medical billing practices, physicians must implement a well-organized system with precise attention to detail. Accounts receivable (A/R) maintains a direct impact on the financial state of healthcare practices. A/R follow-up represents the systematic tracking method used to handle outstanding insurance claims and patient balances through communication with insurance providers and patients. Healthcare organizations depend on their accounts receivable follow-up staff to track refused claims and perform follow-up actions to maximize insurance company reimbursement. Billowing accounts receivable follow-ups requires clinical billing professionals who possess unique abilities and talent.
Steps of A/R Follow-up
A/R follow-up maintains these steps in the workflow sequence:
Stage 1: Initial Evaluation
The claims listed on A/R aging reports undergo an evaluation process during stage one. A group of individuals looks at the provider’s policy to establish which invoice amounts will not reduce the total balance.
Stage 2: Analysis and Prioritizing
The stages of collectability commence upon two conditions: first, when healthcare providers determine a claim cannot be collected, or second when health insurers fail to honor negotiated contract pricing with treatment providers.
Stage 3: Collection
Claims processing must be verified according to all mandatory billing details and address updates, as well as medical billing requirements, before refiling any claims that fall beneath carrier filing limits. Professional medical bills get generated following the finalization of outstanding claims payments, posting per client guidelines for required specifications, and resulting in patient payment follow-ups. Various organizations follow different steps along their revenue cycle, or their steps overlap at different times. The vital requirement of this process is to finish all necessary steps while obtaining payment on the unsettled debt, at least to some extent.
What Is AR Process In Medical Billing
Success requires the accomplishment of established medical billing receivables collection stages.
- Patient Registration and Insurance Verification: Medical practitioners must obtain all patient identifying information before checking insurance policies for active status. The verification process of correct insurance data enables medical staff to validate the current medical insurance status of patients.
- Charge Entry and Coding: Medical practitioners must assign appropriate medical codes to all treatments during patient completion of care. Claims transform into reimbursement items for insurance companies after medical practitioners apply proper codes to create them. The accuracy of coding determines the entire payment process.
- Claims Submission: Medical health insurance providers receive claims through electronic data submissions with encoding. The EDI software systems provide secure facilities to transmit claims.
Read all about Revenue Codes, EMT & CPT Codes Here!
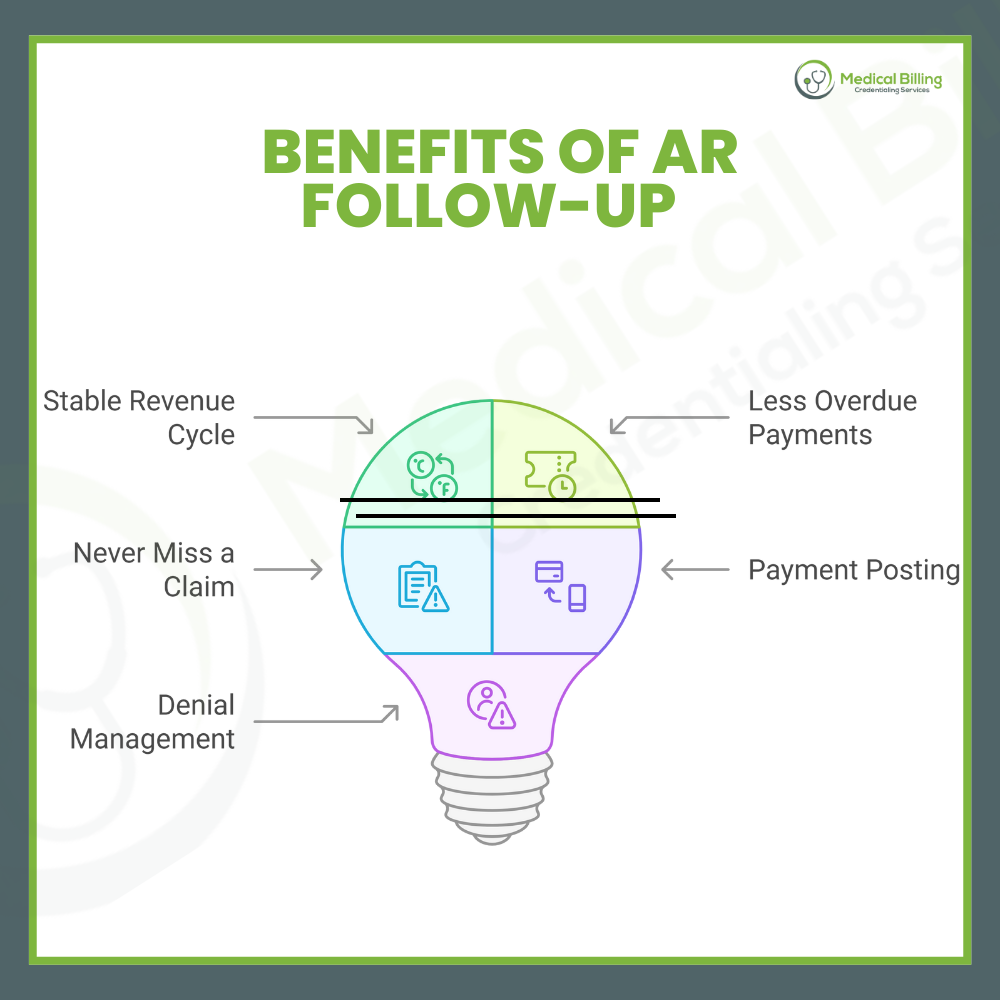
Benefits of A/R follow-up
- Stable Revenue Cycle: A/R follow-up enables the company to receive payments from all clients who have submitted billing requests. The revenue cycle stability enables compensation for physicians’ payments while supporting medical equipment and purchasing supplies.
- Less Overdue Payments: A regular team dedicated to A/R follow-up results in maximum reimbursement collections that decrease the number of overdue payments.
- Never Miss a Claim: The electronic submission of claims allows you to learn about payment approvals and rejections. You should send another request for your claim submission after your initial request gets denied.
- Payment Posting: The insurance claims processing at their company leads providers to obtain either Explanation of Benefits (EOB) or Remittance Advice (RA) documents. Healthcare providers send these documents to insurers to explain the reasons behind claims processing and their reimbursement amounts. The healthcare provider applies received payments straight to patients’ medical accounts.
- Denial Management: Healthcare providers must examine reasons for denied claims through proper investigation before either resubmitting or starting the appeals process. Healthcare providers require effective denial management systems in order to achieve
Best Practices for Managing AR in Medical Billing
Healthcare institutions can use these best practices for AR management and payment delay reduction:
- Regular AR Reports and Reviews: Each organization should check their AR aging reports regularly to find overdue claims so follow-up efforts can be provided proper attention. A regular analysis of payment denials should be followed by solutions to address recurring billing process difficulties.
- Clear and Accurate Billing: Adequate and correct coding, along with precise documentation, must be applied to all submitted claims to prevent denials. Healthcare organizations should maintain updated billing systems that comply with current healthcare laws and regulatory changes.
- Timely Follow-Up: The implementation of specific timeframes needs to regulate interactions between insurance agencies and patient communication. The organization should create its own rules for timing payment follow-up with payers and specify respective actions for expired bill payments.
- Patient Payment Solutions: The practice should welcome patients with various payment alternatives to assist those facing challenges with full bill payment. The first step must include revealing all financial costs to patients before services begin.
- Denials Management and Appeal Process: A formal procedure must exist for accepting and appealing denied payments. Regularly record denial causes for analysis that allows you to modify billing procedures to decrease their frequency.
- Technology and Automation: AR documentation becomes more efficient through software automation which enables resolution management together with payment tracking and automated reminder capabilities. Your patients can find all billing information through patient portals for convenient electronic payments using those portals.
Conclusion
Medical billing needs Accounts Receivable (AR) as a central element that determines healthcare provider financial success. Healthcare organizations that implement proper AR management enhance their financial position by reducing payment delays and improving cash flow together with prompt service payment. Medical billing AR management includes three phases such as claim submission followed by payment posting before performing follow-up and denying claims and patient billing and collections. The optimal management of Accounts Receivable represents a vital knowledge base for medical billing professionals especially Accounts Receivable Specialists who concentrate on streamlining debt collection operations together with debt management activities.
Organizations that implement best practices involving precise billing with immediate follow-up tasks and proficient denials handling techniques coupled with technological solutions will enhance their AR operations and create a stable revenue cycle with increased profitability.
FAQs:
What is the term for the money owed to the medical practice for services provided?
Medical practices receive their service payments under the term accounts receivable (A/R).
A business’s accounts receivable represent the complete monetary value that customers must pay for products and services delivered without payment. The medical practice has a money obligation that reflects the patient and insurance company’s responsibilities for payment of medical treatments.
What does AR mean in medical billing?
In medical billing, AR stands for Accounts Receivable. Healthcare providers receive their outstanding payments as receivable amounts from both patients and insurance organizations for medical services. Managing AR demands monitoring unpaid balances while performing follow-up procedures and collecting payment amounts from those balances. The proper management of AR accounts proves essential to keep healthcare organizations financially solvent while sustaining their cash flow operations.
What does AR stand for billing?
Healthcare organizations use Accounts Receivable (AR) as their terminology for unpaid invoices in billing procedures. The money that patients or clients need to pay a business or organization for received products and services before payment completion represents Accounts Receivable. Medical billing utilizes AR to indicate the total amount of services patients and insurance companies fail to pay.
What is AR in medical terms?
The medical usage of AR indicates either Augmented Reality or Acute Respiratory based on the given circumstance.
- Healthcare professionals use augmented reality technology for medical training, surgery assistance, and patient care through real-time visual overlays of digital healthcare data with physical surroundings.
- The definition of augmentation reality is less popular in medical terminology due to the fact that augmentation reality means acute respiratory conditions.
What does AR stand for in healthcare?
Within the healthcare field, Accounts Receivable stands for AR as its primary meaning. Healthcare providers receive financial compensation through Accounts Receivable, which represents medical service payment duties owed by patients and insurance companies. Healthcare organizations require efficient management of their accounts receivable function to sustain healthy financial cash flow.

